When the threat of the novel coronavirus first emerged, hospitals across the country held meetings to discuss the possibility of the virus attacking their communities and how they would react. Dr. Carla Schwalm ’00 (biology and chemistry), a pediatric oncologist and medical director for her department in the Bronson Medical Group in Kalamazoo, Michigan, kept up with the news and medical reports from other countries that were experiencing coronavirus outbreaks prior to the United States. She participated in a system-wide group of officials who were tasked with making policy for the hospital. “We really feared that our country would be ravaged like Italy was,” she said.
Much of America transitioned to some form of remote work during the spring and summer of 2020, but for the many Greyhound alumni working in healthcare, that was not an option. The COVID-19 pandemic would present these healthcare professionals with the most challenging circumstances of their careers.

Dr. Joseph Smith ’03 (biology and chemistry), section chief of Pulmonary and Critical Care at Eskenazi Health in Indianapolis, shared a similar experience. “In late January, I attended a meeting regarding preparation for an ‘infectious surge,’” he said. “A major topic of this meeting was ventilator allocation, and the discussion of how to distribute those in a time of resource scarcity.”
It was at these meetings that many healthcare providers had to begin considering the allocation of their resources and what they would do when those resources became strained.
“Many hospitals across the country had documents of what to do when we ran out of ventilators,” Dr. Schwalm said. “Thank goodness we didn’t have to use that document, but being a part of that planning was a very emotional time.”
Dr. Smith became consumed with planning after that initial preparatory meeting. “It was at that point everything changed for me,” he said. “How would I find enough doctors to care for a surge of patients in the medical intensive care unit (MICU)? Will we have enough medical supplies, medical devices, monitors, and patient rooms?”
All of the “worst-case scenario” planning was beginning to take a toll on healthcare providers everywhere. “I went to school to save lives, not to determine which ones couldn’t be saved,” Dr. Schwalm said.
According to Dr. Smith, hospital leaders have had to make difficult decisions regarding rationing and reuse of personal protective equipment, working with less capable mechanical ventilators, unsustainable nurse-to-patient ratios, medication shortages, and more. “We’ve been faced with repeated decisions between ‘bad option 1’ and ‘bad option 2,’” he said. “Options that we would have never considered reasonable pre-COVID-19.”
By mid-March, northern states were seeing an uptick in cases, and the doctors went from planning to action. The day-to-day roles of Schwalm and Smith changed dramatically at that point. Schwalm had the difficult task of determining whether COVID-19 or pre-existing cancer was the larger threat to her patients. She also had to find new ways to communicate remotely and conduct her many meetings as a leader in her hospital.
Smith was responsible for his MICU’s agile response to treating COVID patients. “We had to have an accurate number of available mechanical ventilators, a plan to use them, and all of the necessary supplies,” he said. “Alongside our Infection Prevention and Control leaders, we determined the safest way to care for, transport, and even do procedures on patients with COVID-19.”
In addition to well-publicized problems relating to resource scarcity, the doctors have also struggled with having a relatively minimal knowledge of an ever-changing virus. “We were caring for patients by day and scouring newly published data by night,” Smith said.
Dr. Schwalm, who works in pediatrics, has also had to deal with adjusting to new information as it became available. At first it was thought that COVID-19 did not dramatically impact children, so her focus remained on the oncology treatments. “Now with more information emerging about multisystem inflammatory syndrome in children post-COVID, I feel like I’m back at the starting point,” she said. “We are all just doing the best we can with the information that we have.”
I’ve always known that ‘teams’ in hospitals is the only way to practice medicine, but it has become even more important during this time. That includes all of the healthcare workers, not just doctors and nurses.
Dr. Carla Schwalm ‘00
The doctors find themselves struggling with the far-reaching emotional impact of the pandemic as well. Dr. Schwalm noted reduced hospital visitation policies in an effort to reduce the spread of the virus. “The devastation that it has caused families is immeasurable,” she said. “It is so, so hard telling a patient who is going to be in the hospital for a long time that their friends or extended family cannot come to visit.”
Dr. Smith has been deeply moved by the families and friends he has watched say goodbye to a dying loved one via video, and the fear in a patient’s eyes when he was informed he would have to be put on a ventilator. “He told me his wife was on a breathing machine at another hospital,” he said. “These heartbreaking scenarios are far too common today.”
Doctors like Smith and Schwalm have also dealt with the mental stress of their own mortality, and the possibility of taking the virus home to their families. “I have cared for patients much younger and with fewer comorbid conditions than myself,” Smith reflected, thinking of his wife and two children at home. Fortunately, Smith and his family have remained healthy throughout the pandemic but the possibility is never far from his mind.
Despite it all, the harrowing experience has reinvigorated the doctors and also provided them with new perspectives. “I’ve always known that ‘teams’ in hospitals is the only way to practice medicine,” Schwalm said, “but it has become even more important during this time. That includes all of the healthcare workers, not just doctors and nurses.”
Dr. Smith echoed those sentiments, saying that the circumstances have forced his team to find inspiration in the dedication of all the people playing a critical role in the fight against COVID-19. “I work with the most amazing people, at the most amazing facility,” he said. “We’ve found ourselves having to choose the ‘least bad’ option but then still working as a multidisciplinary team to continue to ensure the highest quality of care for our patients.”
Dr. Schwalm hopes that going forward we will all extend one another a bit of grace. “People you encounter are all concerned about different things right now,” she said. “Always in life, but especially now, see past what you see.”
Even though it’s been an extraordinarily difficult time, Dr. Smith has found a positive that can help him get through even the darkest of days. “My confidence in our collective humanity has been heightened,” he said, “While fear and division may have continued to partially shape the headlines, my immediate experience in our local community has been one of unity and cooperation.”
New Greyhounds in Medicine
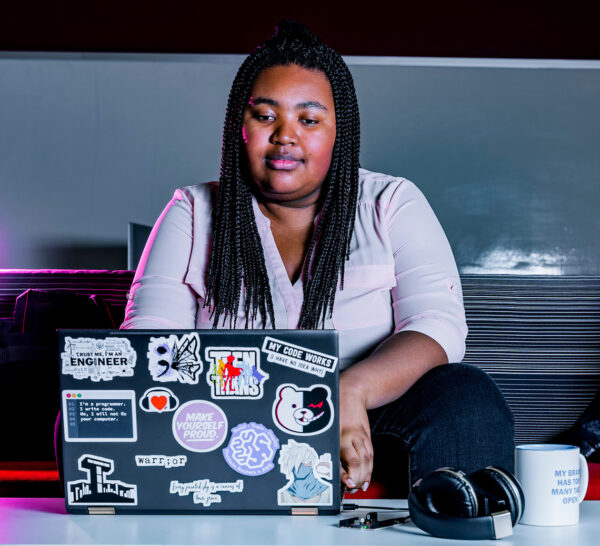
These University of Indianapolis alumni are pursuing careers in medicine. Sofia Gonzalez ’12 (biology and chemistry) received her medical degree from the Universidad Autonoma de Guadalajara in 2019 and begins her residency this year. Mikia Davis ’19 (M.S., anatomical sciences) will begin her studies at Marian University’s College of Medicine in Fall 2020.

I am beyond excited and anxious to start but also a little nervous, as anyone would be. I didn’t think this was how I would be starting residency. I am at a county hospital and know many people affected by COVID are of lower socioeconomic status and with so many uninsured or unable to receive adequate care, we are failing as a health system. I know I will face many challenges in helping care for COVID patients, but I am ready to learn and to help care for my community.
Sofia Gonzalez ’12

I feel really prepared and excited to be starting medical school in the fall. UIndy gave me the confidence, a new skill set, and the resources I needed to prepare myself for the next steps. I’ve been reviewing some of the information I learned during my graduate program in order to prepare myself further and keep the information fresh. Being at UIndy truly gave me the opportunity to prove to medical schools that I was ready when trying to boost my application.
Mikia Davis ’19